Тренутно се преломи дисталног радијуса лече на различите начине, као што су гипсана фиксација, инцизија и редукција унутрашње фиксације, спољашња фиксација носачем итд. Међу њима, фиксација палмарном плочом може постићи задовољавајуће резултате, али нека литература наводи да је стопа компликација чак 16%. Међутим, ако се плоча правилно одабере, стопа компликација се може ефикасно смањити. Дат је кратак преглед врста, индикација и хируршких техника палмарне фиксације за преломе дисталног радијуса.
I. Врсте прелома дисталног радијуса
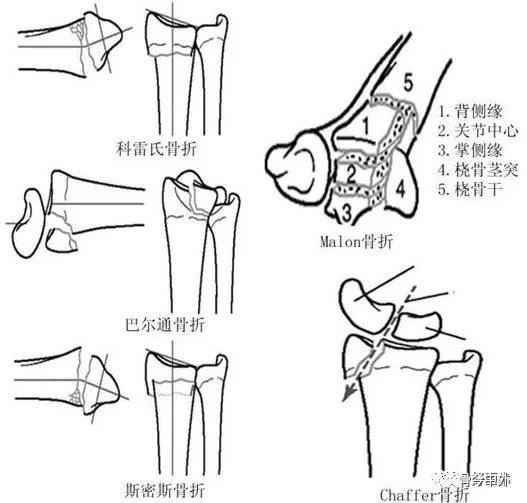
Постоји неколико система класификације прелома, укључујући Милерову АО класификацију засновану на анатомији и Фемандезову класификацију засновану на механизму повреде. Међу њима, епонимска класификација комбинује предности претходних класификација, покрива четири основне врсте прелома и укључује Малеонове четвороделне преломе и Шаферове преломе, што може бити добар водич за клинички рад.
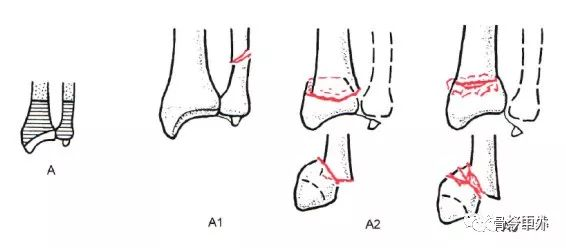
1. Милерова АО класификација - парцијални интраартикуларни преломи
АО класификација је добро прилагођена преломима дисталног радијуса и дели их на три главна типа: екстраартикуларни прелом типа А, делимични интраартикуларни прелом типа Б и тотални прелом зглоба типа Ц. Сваки тип је даље подељен на различите комбинације подгрупа на основу тежине и сложености прелома.
Тип А: Екстраартикуларни прелом
А1, прелом улнарног фемура, радијус као повреда (А1.1, прелом улнарног стабла; А1.2 једноставан прелом улнарне дијафизе; А1.3, коминутивни прелом улнарне дијафизе).
А2, Прелом радијуса, једноставан, са уметком (А2.1, радијус без нагиба; А2.2, дорзални нагиб радијуса, тј. Путо-Колесов прелом; А2.3, палмарни нагиб радијуса, тј. Гојранд-Смитов прелом).
А3, Прелом радијуса, уситњен (А3.1, аксијално скраћивање радијуса; А3.2 клинасти фрагмент радијуса; А3.3, уситњени прелом радијуса).
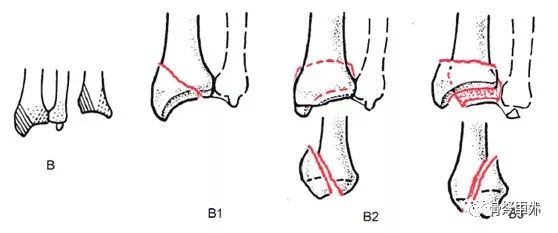
Тип Б: делимични прелом зглоба
Б1, прелом радијуса, сагитална раван (Б1.1, латерални једноставни тип; Б1.2, латерални коминутивни тип; Б1.3, медијални тип).
Б2, Прелом дорзалног обода радијуса, тј. Бартонов прелом (Б2.1, једноставан тип; Б2.2, комбиновани латерални сагитални прелом; Б2.3, комбинована дорзална дислокација зглоба).
Б3, Прелом метакарпалног обода радијуса, тј. анти-Бартонов прелом или прелом типа II по Гојранд-Смиту (Б3.1, једноставно фемурално правило, мали фрагмент; Б3.2, једноставно прелом, велики фрагмент; Б3.3, уситњени прелом).
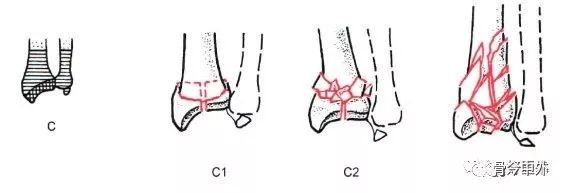
Тип Ц: тотални прелом зглоба
Ц1, радијални прелом са једноставним типом и зглобних и метафизних површина (Ц1.1, задњи медијални зглобни прелом; Ц1.2, сагитални прелом зглобне површине; Ц1.3, прелом короналне површине зглобне површине).
Ц2, Прелом радијуса, једноставна артикуларна фасета, уситњена метафиза (Ц2.1, сагитални прелом артикуларне фасете; Ц2.2, прелом короналне фасете артикуларне фасете; Ц2.3, артикуларни прелом који се протеже у радијално стабло).
Ц3, радијални прелом, уситњен (Ц3.1, једноставан прелом метафизе; Ц3.2, уситњени прелом метафизе; Ц3.3, зглобни прелом који се протеже до радијалног стабла).
2. Класификација прелома дисталног радијуса.
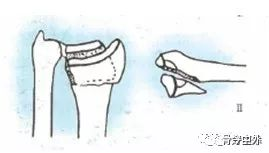
Према механизму повреде, Фемандезова класификација се може поделити на 5 врста:.
Преломи типа I су екстраартикуларни метафизни уситњени преломи као што су Колесови преломи (дорзална ангулација) или Смитови преломи (метакарпална ангулација). Кортекс једне кости се ломи под напоном, а контралатерални кортекс се уситњава и угњетњава.
Прелом
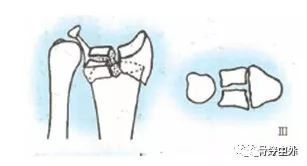
Преломи типа III су интраартикуларни преломи, узроковани смицајним напоном. Ови преломи укључују палмарне Бартонове преломе, дорзалне Бартонове преломе и преломе радијалног стабла.
Смичући напон
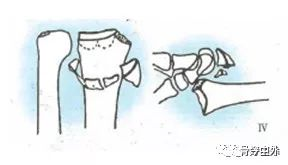
Преломи типа III су интраартикуларни преломи и метафизне инсерције узроковане компресионим повредама, укључујући сложене артикуларне преломе и преломе радијалног пилона.
Уметање
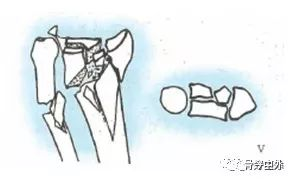
Прелом типа IV је авулзиони прелом лигаментног припоја који настаје током прелома-дислокације радијалног карпалног зглоба.
Авулзиони прелом I дислокација
Прелом типа V настаје услед повреде великом брзином која укључује вишеструке спољашње силе и опсежне повреде. (Мешовито I, II, IIII, IV)
3. Епонимско куцање
II. Лечење прелома дисталног радијуса палмарном плочом
Индикације.
За екстраартикуларне преломе након неуспеха затворене репозиције у следећим условима.
Дорзални угао већи од 20°
Дорзална компресија већа од 5 мм
Скраћивање дисталног радијуса веће од 3 мм
Померање дисталног блока прелома веће од 2 мм
За интраартикуларне преломе са померањем већим од 2 мм
Већина научника не препоручује употребу метакарпалних плоча за повреде високе енергије, као што су тешки интраартикуларни коминутивни преломи или тежак губитак костију, јер су ови дистални фрагменти прелома склони аваскуларној некрози и тешко их је анатомски репозиционирати.
Код пацијената са вишеструким фрагментима прелома и значајним померањем са тешком остеопорозом, метакарпална плоча није ефикасна. Субхондрална потпора дисталних прелома може бити проблематична, као што је продор шрафова у зглобну шупљину.
Хируршка техника
Већина хирурга користи сличан приступ и технику за фиксирање прелома дисталног радијуса палмарном плочом. Међутим, потребна је добра хируршка техника да би се ефикасно избегле постоперативне компликације, нпр. репозиција се може постићи ослобађањем блока прелома од уграђене компресије и обнављањем континуитета кортикалне кости. Може се користити привремена фиксација са 2-3 Киршнерове игле, итд.
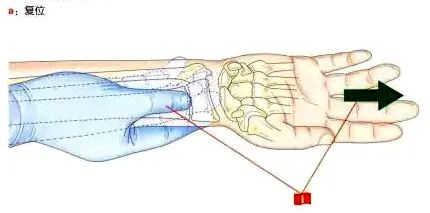
(I) Преоперативно репозиционирање и држање
1. Тракција се врши у правцу радијалног тела под флуороскопијом, при чему палац притиска проксимални блок прелома надоле са палмарне стране, а остали прсти подижу дистални блок нагоре под углом са дорзалне стране.
2. Лежећи положај на леђима, са захваћеним екстремитетом на ручном столу под флуороскопијом.
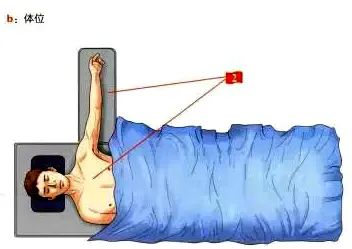
(II) Приступне тачке.
За врсту приступа који ће се користити, препоручује се PCR (радијални карпални флексор) проширени палмарни приступ.
Дистални крај реза коже почиње у набору коже зглоба и његова дужина се може одредити према врсти прелома.
Тетива радијалног флексора карпи радиалиса и њена тетивна овојница се инцизирају, дистално од карпалних костију и проксимално, што је могуће ближе проксималној страни.
Повлачење тетиве радијалног карпалног флексора на улнарну страну штити средњи живац и комплекс тетиве флексора.
Парона простор је изложен, а предњи ротатор ануса се налази између флексора дигиторум лонгуса (улнарна страна) и радијалне артерије (радијална страна).
Направите инцизију на радијалној страни предњег ротаторног мишића, водећи рачуна да део треба оставити причвршћен за радијус за каснију реконструкцију.
Повлачење предњег ротаторног мишића ануса на улнарну страну омогућава адекватнију експозицију улнарног рога на палмарној страни радијуса.

Палмарни приступ открива дистални радијус и ефикасно открива улнарни угао.
За сложене типове прелома, препоручује се да се дистални брахиорадијалисни граничник може отпустити, што може неутралисати његово повлачење на радијални туберозитет, у ком тренутку се може инцизирати палмарна овојница првог дорзалног одељка, што може открићи дистални радијални блок прелома и радијални туберозитет, интерно ротирати радијус Yu да би се одвојио од места прелома, а затим ресетовати интраартикуларни блок прелома помоћу Киршнерове игле. За сложене интраартикуларне преломе, артроскопија се може користити као помоћ у репозицији, процени и фином подешавању блока прелома.
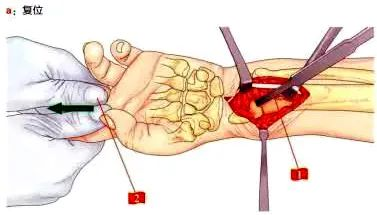
(III) Методе редукције.
1. Користите коштану полугу као полугу за ресетовање
2. Асистент повлачи пацијентов кажипрст и средњи прст, што ће бити релативно лако ресетовати.
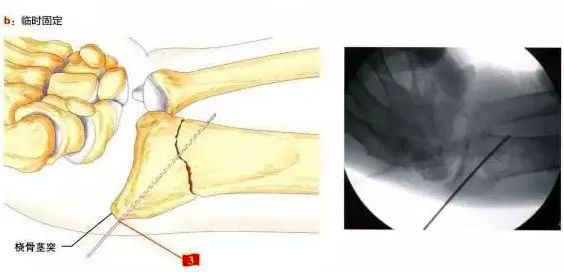
3. Заврните Киршнеров клин из радијалне туберозите за привремену фиксацију.
Након завршетка репозиционирања, рутински се поставља палмарна плоча, која мора бити одмах близу вододелнице, мора покривати улнарну еминенцију и треба да буде проксимално од средишње тачке радијалног стабла. Ако ови услови нису испуњени, ако плоча није одговарајуће величине или ако је репозиционирање незадовољавајуће, поступак и даље није савршен.
Многе компликације су уско повезане са положајем плоче. Ако је плоча постављена предалеко на радијалну страну, вероватно ће се јавити компликације везане за флексор буниона; ако је плоча постављена преблизу линије слива, дубоки флексор прста може бити угрожен. Дислокована деформација прелома која се репозиционира на палмарну страну може лако проузроковати да плоча протрузира на палмарну страну и дође у директан контакт са тетивом флексора, што на крају доводи до тендинитиса или чак руптуре.
Код пацијената са остеопорозом, препоручује се да се плоча постави што ближе линији вододелнице, али не преко ње. Субхондрална фиксација може се постићи коришћењем Киршнерових клинова најближих улни, а Киршнерови клинови и завртњи за закључавање један поред другог су ефикасни у спречавању поновног померања прелома.
Када се плоча правилно постави, проксимални крај се фиксира једним завртњем, а дистални крај плоче се привремено фиксира Киршнеровим клиновима у најулнарнијој рупи. Интраоперативни флуороскопски ортопантомограми, бочни снимци и бочни филмови са елевацијом зглоба од 30° су направљени како би се утврдила репозиција прелома и положај интерне фиксације.
Ако је плоча задовољавајуће позиционирана, али је Киршнеров клин интраартикуларан, то ће довести до неадекватног опоравка палмарне инклинације, што се може решити ресетовањем плоче коришћењем „технике фиксације дисталног прелома“ (Сл. 2, б).
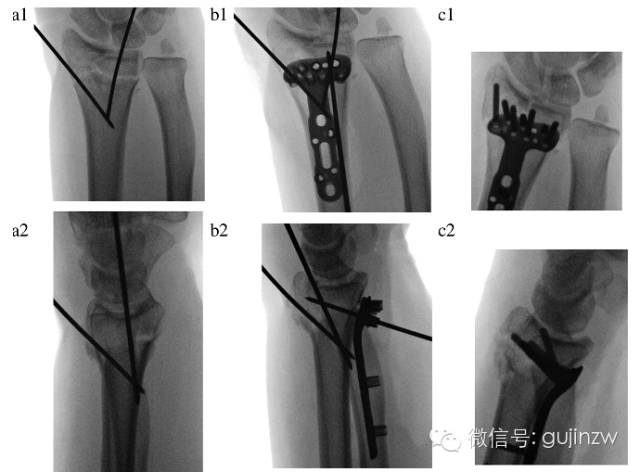
Слика 2.
а, два Киршнерова пина за привремену фиксацију, имајте на уму да метакарпални нагиб и зглобне површине нису довољно обновљени у овом тренутку;
б, Један Киршнеров клин за привремену фиксацију плоче, имајте на уму да је дистални радијус фиксиран у овој тачки (техника фиксације дисталног блока прелома), а проксимални део плоче се повлачи према радијалном стаблу да би се вратио угао нагиба длана.
Ц, Артроскопско фино подешавање зглобних површина, постављање дисталних закључавајућих шрафова/пинова и коначно ресетовање и фиксација проксималног радијуса.
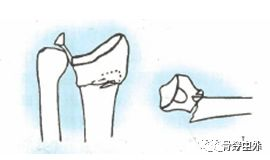
У случају истовремених дорзалних и улнарних прелома (улнарни/дорзални Die Punch), који се не могу адекватно ресетовати затварањем, могу се користити следеће три технике.
Проксимални радијус се ротира антериорно од места прелома, а блок прелома лунаталног дела кости се помера према карпалној кости кроз PCR приступ продужавања; прави се мали рез дорзално од 4. и 5. одељка да би се открио блок прелома, а затим се фиксира завртњима у најулнарнијем отвору плоче. Затворена перкутана или минимално инвазивна фиксација је извршена уз артроскопску помоћ.
Након задовољавајућег репозиционирања и правилног постављања плоче, коначна фиксација је једноставнија и анатомско репозиционирање се може постићи ако је проксимални улнарни клин правилно позициониран и ако у зглобној шупљини нема шрафова (Слика 2).
(iv) Искуство у избору шрафова.
Дужину шрафова може бити тешко прецизно измерити због јаког пригњечења дорзалне кортикалне кости. Шрафови који су предуги могу довести до агитације тетиве, а прекратки да би подржали фиксацију блока дорзалног прелома. Из тог разлога аутори препоручују употребу навојних ексера за блокирање и мултиаксијалних ексера за блокирање у радијалном туберозитету и већини улнарног форамена, као и употребу шрафова за блокирање са танким стаблом у преосталим позицијама. Употреба тупе главе избегава агитацију тетиве чак и ако је навојена дорзално. За проксималну фиксацију плочом за блокирање, за фиксацију се могу користити два завртња за блокирање + један заједнички завртањ (постављен кроз елипсу).
Др Кијохито из Француске представио је своје искуство коришћења минимално инвазивних палмарних блокирајућих плочица за преломе дисталног радијуса, где је њихов хируршки рез смањен на екстремних 1 цм, што је контраинтуитивно. Ова метода је првенствено индикована за релативно стабилне преломе дисталног радијуса, а њене хируршке индикације су за екстраартикуларне преломе АО фракција типова А2 и А3 и интраартикуларне преломе типова Ц1 и Ц2, али није погодна за преломе Ц1 и Ц2 у комбинацији са интраартикуларним колапсом коштане масе. Метода такође није погодна за преломе типа Б. Аутори такође истичу да ако се овом методом не може постићи добра репозиција и фиксација, потребно је прећи на традиционални метод инцизије и не држати се минимално инвазивног малог реза.
Време објаве: 26. јун 2024.